BLACK RIVER, Australia (AP) — The coroner’s sense of futility was clear, as he investigated the death of yet another Australian killed by prescription opioids.
Coroners nationwide have long urged officials to address Australia’s ballooning opioid addiction, and to create a tracking system to stop people from collecting multiple prescriptions from multiple doctors. Yet even as thousands died, the coroners’ pleas were met largely with silence.
“For what it is worth, I add my voice to the chorus pleading for urgency,” Western Australia coroner Barry King wrote in his report, delivered in May.
Half a world away, Australia has failed to heed the lessons of the United States, and is now facing skyrocketing rates of opioid prescriptions and related deaths. Drug companies facing scrutiny for their aggressive marketing of opioids in America have turned their focus abroad, working around marketing regulations to push the painkillers in other countries. And as with the U.S., Australia’s government has also been slow to respond to years of warnings from worried health experts.
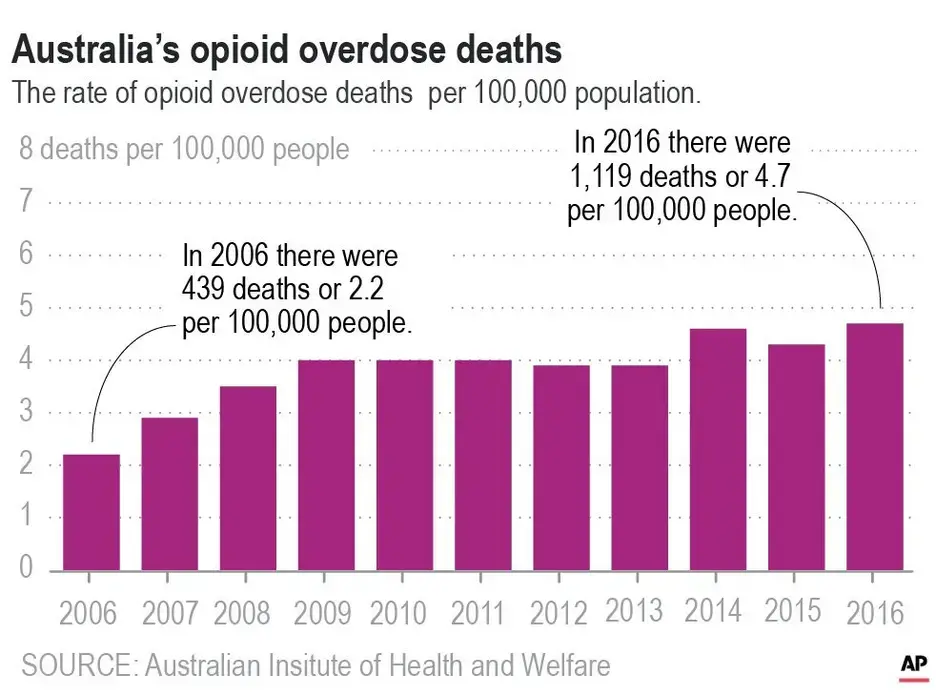
In dozens of interviews, doctors, researchers and Australians whose lives have been upended by opioids described a plight that now stretches from coast to coast. Australia’s death rate from opioids has more than doubled in just over a decade. And health experts worry that without urgent action, Australia is on track for an even steeper spike in deaths like those seen in America, where the epidemic has left 400,000 dead.
“If only Australia could understand how quickly this can get out of hand. We’re not immune to it,” says Jasmin Raggam, whose brother Jon died in 2014 of an opioid overdose and whose brother-in-law is now addicted to the opioid OxyContin. “I was screaming from the mountaintops after Jon died and I’d started doing my research. And it was like I’m screaming and nobody wants to hear me.”
On an island off the coast of Tasmania, Dr. Bastian Seidel and his colleagues are immersed in what he calls a “nightmare scenario.” Two years ago, when he was president of the Royal Australian College of General Practitioners, Seidel dubbed Australia’s opioid problem a “national emergency.” Today, he wonders if anyone was listening.
“It’s depressing at times to see how we, as practitioners, literally messed up our communities,” he says. “It’s our signature on the scripts. ... But the pressure being put on by the drug companies, by certain health sectors — that’s the situation that we are facing now.”
Australia knows the extent of the problem, he says. The country knows addiction is devastating its communities. And yet, he says, nobody is doing anything.
“Unfortunately, in Australia, we’ve followed the bad example of the U.S.,” he says. “And now we have the same problem.”
Australia's Opioid Addiction
Opioids were once reserved for treating pain that was short-term, terminal or related to cancer. But in the 1990s, pharmaceutical companies began aggressively marketing them for chronic pain.
Starting in 2000, Australia began approving and subsidizing certain opioids for use in chronic, non-cancer pain. Those approvals coincided with a spike in opioid consumption, which nearly quadrupled between 1990 and 2014, says Sydney University researcher Emily Karanges.
Dr. Jennifer Stevens, a pain specialist, saw the surge with startling clarity while working at St. Vincent’s Hospital in Sydney.

A few years ago, a pharmacist at the hospital told her they needed to hire an extra person just to handle all the prescriptions they were handing out for Endone, a brand of oxycodone. Stevens discovered that the hospital’s Endone prescriptions had increased 500 percent in 8 years, with no decrease in other opioids dispensed. Further study revealed that 10 percent of patients were still taking opioids three months after surgery, even though the drugs are generally only recommended for short-term use.
“We were just pumping this stuff out into our local community, thinking that that had no consequences,” says Stevens, a vocal advocate for changing opioid prescribing practices. “And now, of course, we realize that it does have huge consequences.”
Just like in the U.S., as opioid prescriptions rose, so did fatal overdoses. Opioid-related deaths jumped from 439 in 2006 to 1,119 in 2016 -- a rise of 2.2 to 4.7 deaths per 100,000 people, according to the Australian Institute of Health and Welfare. Most of those deaths were related to prescription opioids, rather than illegal opioids such as heroin.
More than 3 million Australians - an eighth of the country’s population - are getting at least one opioid prescription a year, according to the latest data.
The numbers and the warnings may have been glossed over partly because of Australia’s piecemeal system of data collection and reporting, says Dr. Christian Rowan, an addiction specialist in the state of Queensland. Data is reported by various states, coroners and agencies, and often includes only prescriptions filled through the government-subsidized drug system and not private prescriptions.
“Because it’s fragmented, people haven’t had a line of sight as to what’s happening,” he says.
Australia’s government insists it is now taking the problem seriously. The opioid codeine, which used to be available over the counter, was restricted to prescription-only in 2018. And last month, the country’s drug regulator, the Therapeutic Goods Administration, announced tougher opioid regulations, including restricting the use of fentanyl patches to patients with cancer, in palliative care, or under “exceptional circumstances.”
“I can’t speak for the past,” says Greg Hunt, who became the federal Health Minister in 2017. “I can speak for my watch and my time where this has been one of my absolute priorities, which is why we’ve taken such strong steps. ... My focus has been to make sure that we don’t have an American-style crisis.”
But for Sue Fisher, whose 21-year-old son Matthew died in 2010 of an overdose, it’s too little, too late. The crisis is here, along with what she calls a “crisis of ignorance.”
“We’re living in a country that is oblivious to what’s going on,” she says. “Why aren’t we learning from America’s mistakes? Why don’t we learn?”
The Drug Companies
When Rustie Lassam thinks of the drug companies that pumped opioids into Australia’s market, she thinks of her infant son’s agonized wails as he went through withdrawal.
For years, doctors had told her that opioids would help her back pain, which led to an all-consuming addiction. During her pregnancy, she swallowed nine high-dose OxyContin tablets every day. So when she thinks about the way pharmaceutical companies have marketed those drugs to doctors, she weeps with rage and grief.
“If only they knew what addiction did to people, how really it affects us to the very core of who we are,” she says. “And there they are, making all this money off the back of my broken life.”
In the U.S., drug companies such as OxyContin maker Purdue Pharma are facing more than 2,000 lawsuits accusing them of overstating the benefits of opioids, downplaying their addictiveness and encouraging doctors to prescribe the drugs to more patients in higher amounts.
In Australia, pharmaceutical companies by law cannot directly advertise to consumers, but are free to market the drugs to medical professionals. And they have done so, aggressively and effectively, by sponsoring swanky conferences, running doctors’ training seminars, funding research papers, giving money to pain advocacy groups and meeting with doctors to push the drugs for chronic pain.
“If the relevant governing bodies had ensured that the way the product was being marketed to doctors especially was different, I don’t necessarily think we would see what we’re seeing now,” says Bee Mohamed, who until recently was the CEO of ScriptWise, a group devoted to reducing prescription drug deaths in Australia. “We’re trying to undo ten years of what marketing has unfortunately done.”
Mundipharma, the international arm of Purdue, has received particular criticism for its marketing tactics in Australia. In 2018, addiction specialist Dr. Simon Holliday filed a complaint against the company over a marketing pamphlet for its drug Targin, a painkiller designed to prevent the constipation that is common with other opioids.
The brochure cited 2009 guidance from the Royal Australian College of General Practitioners that says weak opioids are less effective than strong ones. But in a statement, the doctors’ group said the ad was misleading and that Mundipharma appeared to have deliberately ignored its updated clinical guidelines.
Holliday filed a complaint with Medicines Australia, the pharmaceutical industry’s regulator. But membership to Medicines Australia is not mandatory, and Mundipharma declined to participate in the complaints process because it had dropped out as a member.
Holliday then went to the Therapeutic Goods Administration. He got nowhere. So he wrote to Hunt, the health minister, and other lawmakers. He received no response.
In a statement to The Associated Press, Mundipharma said that the guidelines it referenced were current at the time the pamphlet was in circulation. “The material was balanced, accurate, fully supported by the product information, consistent with the approved indication, and contained adequate safety information,” the company said.
This year, Mundipharma has faced scrutiny over a promotional campaign that critics say violates the spirit of Australia’s law banning drug marketing to consumers.
The campaign, which encouraged people suffering painkiller-induced constipation to talk to their doctors, never mentions Targin by name, because it legally can’t. But the advertising agency Mundipharma hired described on its website how they worked around that regulation, by using print, radio and online ads to target regions where pain medication use was high. Google search data showed that people looking for information on constipation from painkillers used terms like “blocked up,” so the agency used the phrase “blocked pipes.”
In a statement, Mundipharma said the campaign was a “disease awareness initiative” that did not violate the spirit of any law and did not market any medication.
In an interview, Hunt said he has asked the country’s drug regulator, the TGA, to investigate both marketing campaigns, along with some of Mundipharma’s other activities in Australia. Among those activities: the company’s “Pain Management Master Classes” for doctors. The classes, which have provided training to more than 5,000 doctors in Australia, have been praised by some as helpful for physicians seeking guidance on treating complex pain, and condemned by others as a conflict of interest, given they are run by a company that sells painkillers.
Mundipharma said the classes cover non-opioid treatment options and “strongly emphasize” that opioids are only appropriate after a comprehensive assessment.
Stevens, the Sydney pain specialist, has pushed back against several drug companies over their marketing tactics. A couple years ago, she says, Mundipharma was marketing Targin to surgeons at her hospital, reassuring them that they could prescribe higher doses. Unlike pain specialists, surgeons are generally not well-educated on the intricacies of opioids, she says.
Stevens complained to Mundipharma and they stopped the practice. She says they have become much more cooperative since.
“Marketing, on the whole, is very clever and very successful — otherwise it wouldn’t be done,” she says. “We love a freebie. ... We’re no different from other members of the population. It’s just that we are targeted more.”
In a statement, Mundipharma said it strictly adheres to the Medicines Australia code of conduct and has always been transparent about the risks associated with opioids. Still, in a submission last year to the TGA as it considered tougher restrictions on opioids, Mundipharma appeared to minimize the severity of Australia’s problem.
“We acknowledge that there is an issue associated with opioid misuse,” the company wrote. “However to describe the Australian situation as a ‘crisis’ is alarmist and risks stigmatizing patients who have a legitimate need for opioid analgesics to manage their pain.”
How the Government Fell Short
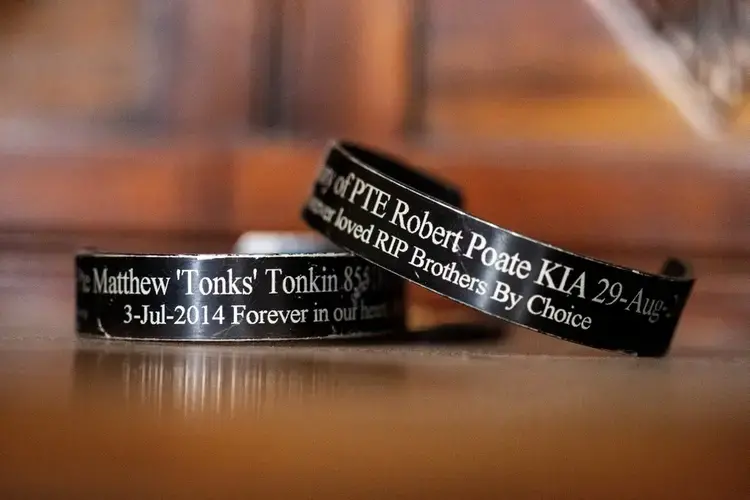
David Tonkin blames his son’s death on a system that allowed him to see 24 doctors and get 23 different medications from 16 pharmacies — all in the space of six months. Between January and July 2014 alone, Matthew Tonkin got 27 prescriptions just for oxycodone.
The addiction that ultimately ended Matthew’s life began in 2012, after he was injured while serving with the Australian army in Afghanistan. When the 22-year-old arrived on leave at his father’s home in the western Australian city of Perth, he held up a stack of OxyContin pill strips. The drugs had been prescribed to him by American doctors in Afghanistan for his injured hip and ankle.

“Look, Dad,” he said. “The Yanks really know how to look after you.”
Matthew was 14 kilograms (30 pounds) lighter than the last time his father had seen him. He was suffering from post-traumatic stress disorder from the horrors of Afghanistan, including the death of his best friend, a fellow soldier. He was also suffering from a growing addiction to opioids. The addiction escalated after the army sent him to recover in Queensland, where doctors put him on an opioid called tramadol.
Matthew soon discovered how easy it was to get whatever prescriptions he wanted. He forged his doctor’s signature. He told one doctor he’d knocked a bottle of pills into the toilet and needed more.
In August 2013, another doctor prescribed him more oxycodone after Matthew said he was suffering from PTSD and hip pain.
A few weeks later, Matthew had his first oxycodone overdose. A few months after that, he was discharged from the army.
One doctor called a hotline for medical professionals to report Matthew’s apparent misuse of prescription drugs. But when Matthew moved back to Perth to live with David, doctors there had no way of knowing his drug use had been flagged in Queensland.
He hopped around clinics collecting prescriptions for opioids. The doctors were largely oblivious to what he was doing because Australia has no national, real-time prescription tracking system.
David begged Matthew’s doctors and pharmacists to stop giving him OxyContin. Matthew just went to other doctors.
At a solemn gathering to honor military personnel on April 25, 2014, two of Matthew’s friends had to hold him upright.
Back at home after the service, David told Matthew to hand over his pills. Matthew shoved David across the kitchen into the cupboard. Then he pinned his father to the floor and began to choke him.
David thought he was going to die.
Matthew eventually let go and both men went to the hospital for treatment. Two days later, Matthew called his father. “Do you still love me, Dad?” he asked.

And of course, he did. So David kept trying to save him, right up until July 3, 2014, when he returned home from a walk and realized Matthew hadn’t come out of his room all morning.
The night before, Matthew had been sick. David had cleaned the vomit off his son’s bedroom floor and changed his sheets. Matthew took a shower, thanked his father and climbed into bed.
David walked into his son’s room. “Time to get up, mate.”
There was no answer.
David placed a hand on Matthew. His body was warm. But he had no pulse.

David called for an ambulance and started CPR. As he pumped his son’s chest, the dispatcher counted out the beats.
One. Two. Three. Four.
Nothing. Nothing. Nothing. Nothing.
Five. Six. Seven. Eight.
Nothing.
Warnings Ignored
The conclusion from King, the coroner, was blunt: Had a prescription tracking system been in place, Matthew would not have been given the oxycodone that killed him.
King’s findings on Matthew’s death were delivered at least a dozen years after the first coroners’ reports began warning of a growing opioid problem. As early as 2007, a coroner had suggested that someone look into why the opioid prescription rate on the island of Tasmania was so high.

Two states — Tasmania and Victoria — developed their own prescription tracking systems, but they only monitor opioid prescriptions within their respective states, and neither is currently mandatory.
The development of a national system has been mired in bureaucratic delays. In 2017, the government committed 16 million Australian dollars (US$11 million) to creating one, and Hunt, the health minister, later said it would be ready by the end of 2018. It has yet to be rolled out.
In an interview, Hunt blamed the delay on the states. The national framework is ready, he said, but the states must connect to it.
In March 2019, New South Wales coroner Harriet Grahame warned that Australia’s opioid deaths could reach many thousands over the next five years.
“We appear to have few coordinated strategies to address this problem,” Grahame wrote in a report. “Lowering the rate of opioid overdose is clearly achievable but it will require a government willing to listen to health experts and to act decisively on their advice.”
After Matthew died, and for years to come, David would suddenly awaken at 10 p.m. — the same time that Matthew used to call from Afghanistan. Now, instead of his son’s voice, there is only silence.
The Poor Pay the Price
From her home in rural northwest Tasmania, 51-year-old Carmall Casey seethes over a system she says pushed her and so many others into addiction. It is a system that has made opioids the cheap and easy alternative for Australians, particularly the poor.
“I became an addict without knowing,” Casey says.
Here in Tasmania, there are echoes of American Appalachia — in the rural towns, the poverty and the cascade of lives torn apart by pills that promised to take away the pain but in the end created more.
This is Australia’s poorest state, and like Appalachia, it is the country’s epicenter for opioids. Tasmania has the nation’s highest rate of opioid packs sold per person — 2.7 each. One region has the highest number of government-subsidized opioid prescriptions in Australia: more than 110,000 for every 100,000 people.
Ten years ago, while working as a dairy farmer, Casey jumped off a truck and felt her knees give way. An operation provided temporary relief, but the pain came back. She was told she had osteoarthritis.
A doctor prescribed her opioids to ease her pain. When she stuck the first patch on her skin, it felt like heaven.
But the agony eventually returned, so the doctor upped the dosage. The side effects were hell — depression, anxiety, panic attacks. And her pain got worse.
Desperate, she saw other doctors. They sent her away with more prescriptions for more opioids: fentanyl, codeine, oxycodone, tramadol, buprenorphine, tapentadol, Targin.
An estimated 20% of Australians suffer chronic pain. But in poor, rural areas, access to pain specialists can be logistically and financially difficult. Wait lists are long, and a few sessions with a physiotherapist can cost hundreds of dollars. Under the government-subsidized prescription benefit plan, a pack of opioids costs as little as AU$6.50 ($4.50.)
Dr. Tim Andrewartha, a general practitioner in northwest Tasmania, says giving a patient with chronic pain a drug for quick comfort can be tempting, when the alternative may be a years-long wait to see a specialist.
“As a medical practice, we’re just falling short in terms of acknowledging the lack of evidence that these drugs have for chronic, long-term use,” he says.
Casey couldn’t afford private health insurance, so finding a surgeon who would treat the cause of her pain was a struggle. She drove ten hours roundtrip to meet a surgeon in the capital, Hobart, only to be told the wait list for the operation was two years.
While taking a truck driving course, she injured her shoulder and began the same carousel of fruitless doctors’ appointments.
She tried to quit the painkillers. She returned them to the pharmacy and dumped them down the sink. She suffered through the nightmares and shakes of withdrawal. But eventually, the pain would grow unbearable, so she’d take the drugs again.

She lost her farm. Even worse, she says, she lost her daughter.
She made bad choices on the drugs, she admits now. She was living with a volatile man who began to bully Sarah, so she sent her daughter, then 14, to live with her father. It’s a decision that tore them apart, and still tears Casey apart today.
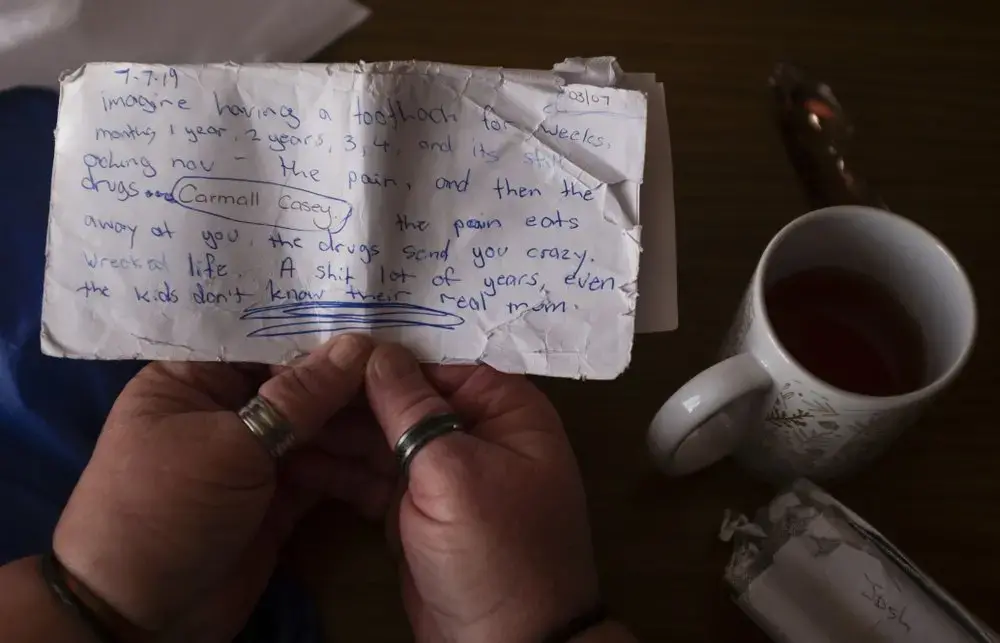
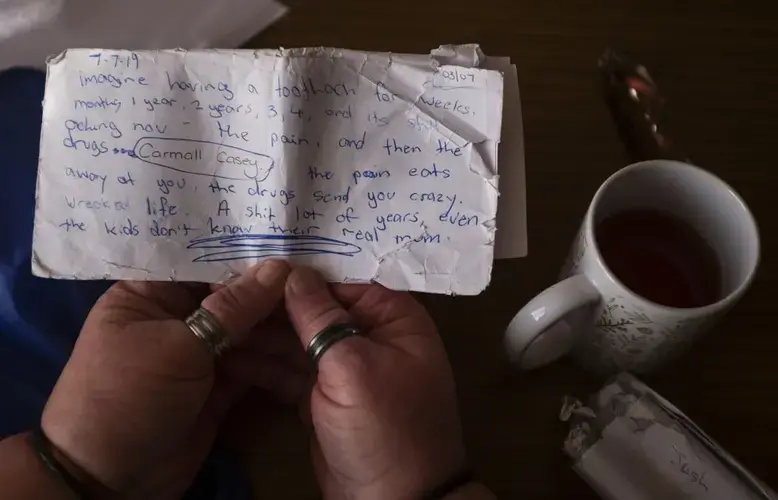
One day, she scrawled her anguish on a tattered envelope. “Imagine having a toothache for weeks, months 1 year, 2 years, 3, 4, and it’s still aching now ... the pain eats away at you, the drugs send you crazy,” she wrote.
In June, she told herself: Enough. She returned the remaining pills to her pharmacist.
She found a surgeon who took her seriously. And she got an appointment with a physiotherapist who is teaching her exercises to manage her pain.

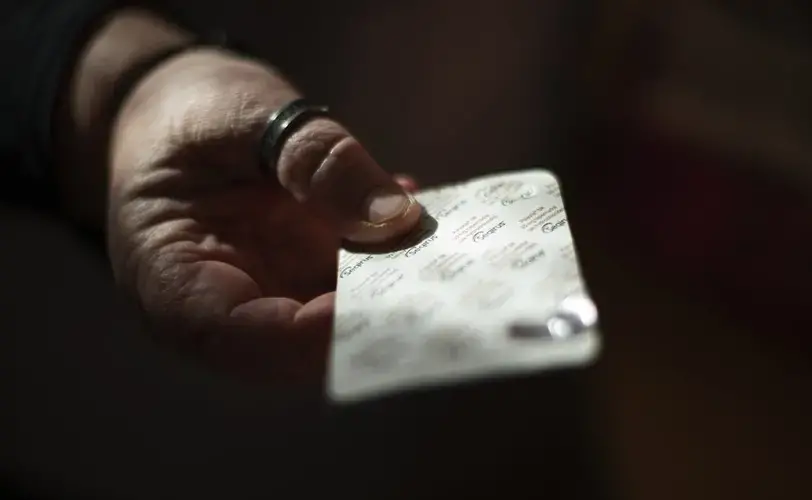
On a recent afternoon, she rifles through a box of medicine in her kitchen. Suddenly, she freezes. Tucked inside is an old pack of tapentadol that she thought she’d thrown away. She washes the pills down the kitchen sink.
She doesn’t know what she’ll do when the pain returns. But she says she will never return to opioids.
“I’m not going back,” she says and begins to weep. “I’m not.”

Education Resource
Meet the Journalist: Kristen Gelineau
The Associated Press is investigating how the opioid epidemic, once thought to be an American...