MUMBAI, INDIA—One day at the end of April, dentist Azmera Shaikh tested positive for the novel coronavirus. That afternoon, feeling feverish and achy, she and her mother, who had also tested positive, descended from their apartment here to board an ambulance to the hospital. They were startled to find a dozen or so neighbors lined up with mobile phones in hand. Pictures and videos of their departure soon circulated on WhatsApp and Facebook. “We were entertainment,” Shaikh says. “We were the joke of the town.”
A volunteer with the nonprofit Doctors for You, Shaikh had seen the fear and distrust brought by the pandemic while working in the slums of eastern Mumbai. Some areas had not allowed her team to set up screening camps for fear that residents would be assumed infected with SARS-CoV-2, the virus that causes COVID-19. But she didn’t expect her educated, middle-class neighbors to behave similarly.
Soon, her entire family was in quarantine. The rules made it difficult for her father and brother to put out garbage and get groceries. Yet neighbors did not help. Their attitude, Shaikh says, was “more traumatizing than the illness itself.”
As the coronavirus spread early this year, people around the world responded in similar ways. In Nepal, health care workers were thrown out of rental apartments. In Haiti, hospitals treating COVID-19 patients were attacked. In the United States, many people avoided East Asian–dominated neighborhoods, linking the virus with people from China, where the outbreak began.
Some doctors in Chennai, India, avoided getting tested because of the trouble they might face with neighbors if they turned out to have the virus, notes medical anthropologist Mitchell Weiss, a professor emeritus at the Swiss Tropical and Public Health Institute. As doctors, they should know better because testing is critical to reducing outbreaks, he says. “This is the toxicity of stigma.”
Yet those responses would have been familiar to our ancestors. From ancient times, humans have feared disease and shunned those thought to have it. But today, when we have a larger arsenal of tools to fight disease, including testing, contact tracing, and treatment, those old responses can undermine public health efforts. Stigma not only encourages people to hide illness and avoid treatment, but also intensifies patient stress and reinforces socioeconomic inequality.
The history of epidemics, including those of leprosy, cholera, and HIV, shows how costly stigma can be—both to individual patients and to societies as a whole. Such costs don’t usually show up in conventional epidemiological studies, Weiss says, but are part of what the World Health Organization (WHO) calls “the hidden burden” of disease.
RELICS OF PAST DISEASES pepper the Indian port city of Mumbai. A 160-year-old temple to Sitladevi, the goddess of smallpox, is still open to worshipers. Nineteenth century crosses to ward off bubonic plague are sprinkled around Catholic neighborhoods. And a sprawling 130-year-old leprosy home still stands in what was once the outskirts of colonial Bombay.
The word “stigma” originally referred to a mark on the body. Later it came to denote a metaphorical mark of disgrace. Sociologists define stigma as the social devaluing of people who possess a trait seen as negative or deviant, such as a physical or mental disability or even an ethnicity. Almost every sense of the term comes together in leprosy.
The association is ancient: The biblical book of Leviticus depicts leprosy as a manifestation of spiritual sin, calling people with the condition “unclean” and directing them to live “outside the camp.” (Biblical leprosy likely referred to other skin conditions, but the diseases were conflated.) In India, where the disease is thought to have originated, ancient Hindu texts proscribed marriage into families that had a member with leprosy. In Europe, people with the disease were cast out of town or sent to leprosariums.
“In infectious disease, stigma is rooted in an exaggerated fear of contamination,” Weiss says. Some psychologists suggest stigma may have developed under evolutionary pressure to protect the social group from infected members. (A similar hypothesis proposes that the emotion of disgust evolved to prevent humans from ingesting pathogens.) Avoiding people with infectious diseases probably did help ancient societies mitigate epidemics, Weiss notes. “In situations of plague or other highly contagious diseases, these fears may not be unreasonable. But how you act on those concerns may become unreasonable or unwarranted.”
History suggests stigma often sweeps beyond realistic concerns about contagion. In the mid to late 1800s, people in the United Kingdom panicked over leprosy, seeing the disease in racist terms, notes medical historian Shubhada Pandya, who is associated with the Acworth Leprosy Museum in Mumbai. An 1862 article in The BMJ said the countries of Asia were “infested” with leprosy “in proportion to the physical and moral degradation of their people.” An 1898 colonial law empowered officials in India to round up and isolate homeless patients in institutions that were often segregated by sex to prevent procreation.
In 1873, Norwegian scientist Gerhard Armauer Hansen isolated the bacterium that causes leprosy. During the mid to late 20th century, researchers developed treatments and the disease became less common. Still, people with leprosy continued to be shunned. Patients themselves internalized the stigma: Just last year, researchers who interviewed residents of a leprosy colony in Ghana reported that even people who were cured preferred to stay in the colony because they were ashamed of their disease and expected to be ostracized at home.
Health-related stigma can sometimes have a “compounding effect” on other kinds of prejudice, exacerbating inequality, says Wim van Brakel, medical director of NLR, an international nongovernmental organization to fight leprosy in Amsterdam. For example, according to a 1996 ethnographic study in Thailand, many older people associated leprosy with begging, probably because in the past, ostracism and disability threw patients with the disease into poverty and eventually begging. A similarly outdated view has shaped perceptions in India. “The image people have is that if I get leprosy, I become like that maimed beggar at the traffic light,” van Brakel says.
The bright spot is that helping people with one aspect of their plight may alleviate others. In a randomized controlled study of leprosy patients in Indonesia from 2011 to 2014, van Brakel found that improving their socioeconomic situation with loans and training helped reduce their perceptions of social stigma and boost their participation in society.
Yet uprooting old views remains a challenge. Even in 2018, a survey of people in Cameroon indicated that one-quarter of 233 respondents believed leprosy was caused by a spell. Most knew the disease was curable, but more than one-quarter said they would not marry someone who had had it. In India, laws making the disease grounds for divorce were removed only last year.
Even the disease’s name has come to mean outcast: We describe those we shun as “lepers.” Scientists tried to change the name to Hansen’s disease, but the old name stuck. Ashim Chowla, former head of the nonprofit Lepra India, says people today still flinch when he tells them he has been treated for leprosy. “The identity never really goes away.”
Chowla, now CEO of the India HIV/AIDS Alliance, admits to some schadenfreude seeing people in his middle-class neighborhood turn on each other today because of COVID-19. Indian elites “who never thought they would get the diseases of the poor,” he says, are getting a taste of “the ostracism that leprosy patients have faced for thousands of years.”
LEPROSY HAS LONG EPITOMIZED the stigma associated with disease. But in the 1980s, a virus emerged that quickly became the new “gold standard of stigma,” Weiss says: HIV. At first, AIDS, the disease caused by HIV, was seen as a health threat largely for gay men, injecting drug users, and sex workers. The initial response was marked by moral panic, similar to old views of leprosy. Some religious groups saw the illness as a curse or punishment. People with the disease faced discrimination and government neglect in most countries, says Laura Nyblade, an expert on HIV discrimination with RTI International.
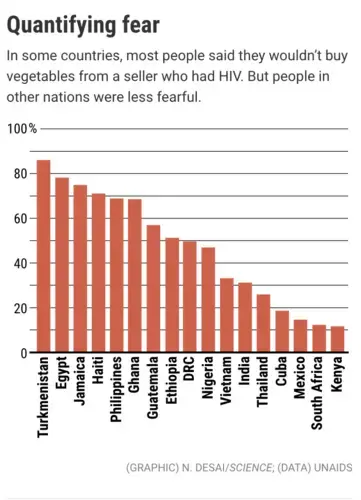
Social scientists like Weiss had used survey and interview methods to measure stigma and discrimination in mental illness and leprosy, creating “stigma scales” to quantify it. With the advance of HIV, researchers began to develop similar scales for that virus. In 2008, the Joint United Nations Programme on HIV/AIDS (UNAIDS) launched the People Living with HIV Stigma Index as a tool to generate evidence for advocacy. By November 2017, more than 100,000 people living with HIV had been interviewed in more than 50 languages by trained interviewers who themselves had HIV. Interviewers asked, for example, whether someone had been insulted for being HIV-positive or been denied access to health care.
Studies showed stigmatization burdened people with HIV psychologically, as Shaikh and her family experienced with the coronavirus. Stigma also caused people to hide their disease, lessened adherence to treatment, and worsened health outcomes. People with HIV who perceived high levels of social stigma were 2.4 times as likely to delay entering care until very ill, according to a meta-analysis of 10 studies published in 2017. One in five people living with HIV avoided going to medical facilities because they feared discrimination, according to data collected from 2011 to 2016 in 19 countries. And University of Washington researchers found in 2019 that Black women living with HIV who scored high on stigma measures also reported more days of missed treatments and higher viral loads.
All those findings suggest stigmatization can spur the spread of disease. In some settings, stigma could be responsible for 35% to 51% of infant infections with HIV because it reduced mothers’ adherence to treatment, according to a 2017 modeling study by Nyblade and colleagues.
People already living at the margins suffer even more. In one study in Russia, 30% of female sex workers said they had been refused medical care because of their work, which puts them at risk of contracting HIV. In a study in Argentina, 40.7% of transgender women, who have higher rates of HIV, said they avoided clinics because of their transgender identity. According to a 2015 survey in New York City, African migrants with undocumented status chose not to disclose HIV status to families and communities, fearing they might lose needed social support. Like other marginalized groups, they “stayed hidden and disengaged with health care,” the study said.
As with leprosy, social attitudes were intensified by legal discriminations that never fully went away. Some aspects of HIV transmission, such as not disclosing that one is infected, are still criminalized in 72 countries, including the United States, according to UNAIDS. Thirty countries ban people’s entry or residence on the basis of HIV status.
“A critical lesson from HIV is that addressing stigma from the outset of a pandemic can be critical to an effective response,” Nyblade says. “If people fear stigma, they will be reluctant to get tested, disclose they have symptoms, and seek care.” More than 30 years after the disease emerged, she says, “stigma continues to be a major barrier to ending the HIV pandemic.”
STIGMATIZATION OFTEN DEEPENS existing fault lines based on class, caste, race, or any “outsider” status. Those dynamics can be self-perpetuating: Marginalized groups who live in crowded conditions with less access to health care are often hit harder by disease—and then are blamed for it.
Migrants are especially vulnerable to vilification. Mary Mallon, an Irish immigrant cook in early 1900s New York City, was dubbed “Typhoid Mary” for being an asymptomatic carrier of the typhoid bacteria. After infecting several wealthy households, where some members died, she was forced into quarantine in a hospital on an island near the city, where, she complained in a letter to her lawyer, she was “a peep show” for visitors. In late 2010, Dominicans blamed migrant workers for a cholera outbreak that began when Nepali peacekeepers inadvertently introduced it to neighboring Haiti. Researchers from Emory University found that Dominicans connected the outbreak to character flaws or unhygienic habits among immigrant Haitians, who faced structural problems including lack of access to safe water and sanitation. One year into the epidemic, the government may have worsened the situation by making it more difficult for immigrants to get the legal status needed for health insurance.
COVID-19, too, may become associated with specific groups, says medical anthropologist Alexandra Brewis-Slade of Arizona State University, Tempe. “It is politically expedient and useful to be able to blame and distract,” giving politicians an excuse for public policy failures, she says. Stigmatization “discourages investment [in combatting disease] because it devalues the people who would benefit most,” she says. “Stigma is often beneficial to those in power.”
Nyblade agrees that “COVID-19 may provide an excuse to further stigmatize already stigmatized groups.” In India, where a Hindu nationalist party is in power, many people targeted an international Muslim conference held in the country in March with the social media hashtag #CoronaJihad. The Bombay High Court recently dismissed police charges filed against attendees for spreading the disease.
Indeed, many incidents in the current pandemic echo familiar patterns of animosity, especially in areas where the coronavirus has newly entered. Apartment dwellers on the outskirts of Mumbai, where COVID-19 cases have been growing, recently tried to throw out resident nurses because of fear that the nurses would bring the virus home. In the Indian state of Karnataka, 35 migrant workers who had returned to their village from Mumbai in June were quarantined. When seven tested positive, the group vanished overnight. “They feared reprisals,” says Edward Premdas Pinto, a public health activist at the Centre for Health and Social Justice who works in the region.
In one rural village, Pinto says, an elderly man returned from the hospital to find that his family had fled the house, fearing his return. He hanged himself. And in the United States, an advocacy group has recorded about 2600 hate-related incidents against Asian Americans between March and August, including spitting, racial slurs, and even assault. Many abusers specifically referred to the coronavirus.
MONTHS AFTER her traumatic experience with her Mumbai neighbors, Shaikh believes attitudes have improved as people have become more familiar with COVID-19. For those working to curb stigma, past pandemics can offer some lessons.
In leprosy and HIV, good information about mode of transmission and available treatments helped improve attitudes. HIV also showed that “sunlight itself can be a cure” for stigma, Weiss says. “Bringing attention to the existence of stigma enables people to [look for] areas where they can make their system function more effectively.” A strong health system is critical, too, say Indian public health activists, because it builds trust in medical authorities.
As seen with leprosy, language matters, which is why WHO in 2015 recommended against using countries, regions, animals, or people when naming viruses. Language remains a flash point with the coronavirus, with U.S. President Donald Trump regularly referring to “the China virus.” In March, some public health experts tried—and failed—to convert the prescription for “social distancing” into “physical distancing” because of the potential connotations of the original phrase in societies riven by class, caste, and ethnicity. (In psychology, the social distance scale is a measure of racial or ethnic prejudice.)
Brewis-Slade cites New Zealand as a model for its “clear leadership, communicated with empathy and compassion.” The country has seen its share of prejudice during the pandemic; East Asians and historically oppressed Pacific Islanders have faced racist comments. But the government has quickly condemned such incidents while explicitly encouraging testing.
“People who we know have tested positive to COVID-19 are to be commended; they have done their bit” to protect others, Ashley Bloomfield, New Zealand’s director of health services, said in a press conference last month. There is “no shame or blame” in being infected with a virus, he said.
Pinto also stresses the importance of balanced media coverage. Indian TV news channels have stoked fear with a singular focus on the rising number of infections, he says. “Talking about recovery rate and success stories would help.” U.S. basketball player Magic Johnson’s 1991 disclosure of his HIV-positive status, for example, helped change public perceptions of the disease.
Hearing from other people in the community can be even more effective than listening to experts or celebrities, Nyblade says. In RTI-led research in Ghana and Tanzania, she and colleagues set up training workshops and other activities in five of 10 selected clinics and then compared attitudes among the health care workers toward people with HIV. Learning from trained peers rather than experts had more impact. “Seeing and hearing people who are ‘just like you’ tell their stories can help dispel myths and misconceptions and break down the ‘othering’ process,” Nyblade says.
That kind of contact may be even more important during an outbreak, when isolation and quarantine are necessary but may compound suspicion. In Mumbai, Shaikh found that community outreach—going door to door with local volunteers and spending time with families—helped change attitudes in the slum where she works. Initially, no one would admit to having symptoms or report their contacts. Now, they’re coming forward to be tested and are more amenable to entering a care facility. A similar approach has helped authorities flatten the curve in Dharavi, one of the city’s largest slums.
The challenge, Shaikh says, is to help people understand that “we have to fight COVID-19 and not COVID-19 patients.”
COVID-19 Update: The connection between local and global issues–the Pulitzer Center's long standing mantra–has, sadly, never been more evident. We are uniquely positioned to serve the journalists, news media organizations, schools and universities we partner with by continuing to advance our core mission: enabling great journalism and education about underreported and systemic issues that resonate now–and continue to have relevance in times ahead. We believe that this is a moment for decisive action. Learn more about the steps we are taking.